Scientists have found ways of culturing organ-specific tissue from stem cells that could change the way diseases are studied and treated.
By Javier Barbuzano
Imagine the possibility of creating individualized, complex collections of cells that bear a resemblance to a patient’s own tissues. That technology—the ability to grow ‘organoids’—is becoming a reality and is finding new uses every day, in part thanks to the work of scientists at the Harvard Stem Cell Institute.
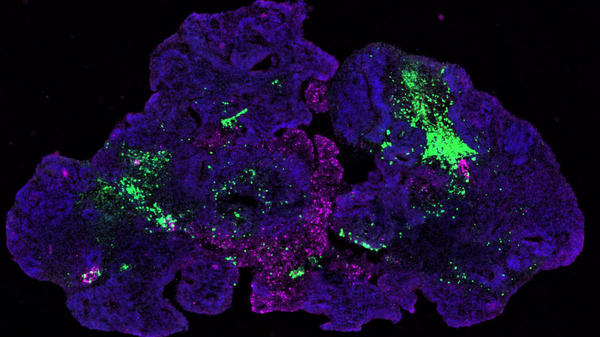
Organoids are tiny, self-organized three-dimensional tissue cultures that are derived from stem cells. Such cultures can be crafted to replicate much of the complexity of an organ, or to express selected aspects of it like producing only certain types of cells.
Organoids grow from stem cells—cells that can divide indefinitely and produce different types of cells as part of their progeny. Scientists have learned how to create the right environment for the stem cells so they can follow their own genetic instructions to self-organize, forming tiny structures that resemble miniature organs composed of many cell types. Organoids can range in size from less than the width of a hair to five millimeters.
There are potentially as many types of organoids as there are different tissues and organs in the body. To date, researchers have been able to produce organoids that resemble the brain, kidney, lung, intestine, stomach, and liver, and many more are on the way.
This way of culturing tissues will give scientists a detailed view of how organs form and grow, providing them with new insights on human development and disease as well as giving them the opportunity to see how drugs interact with these “mini-organs”, potentially revolutionizing the field of drug discovery and opening new approaches to personalized medicine.
Some of these uses are highlighted below in work from four HSCI laboratories.
Understanding ourselves and modelling disease
Most of what we know about embryonic development has been learned by extrapolating to human biology what is observed in mice and other animal models. Now, thanks to organoids, researchers have the possibility of culturing tiny versions of each tissue using human cells.
In the case of the human brain, this technology opens a window to observe some of the most elusive aspects of our own biology. This becomes especially important when trying to study complex, intrinsically human characteristics or diseases. “Some of the most prominent neuropsychiatric or neurodevelopmental diseases of our time, such as schizophrenia or autism spectrum disorder, are uniquely human diseases that affect the whole human genome,” explains HSCI researcher Paola Arlotta, PhD.
Arlotta’s lab developed protocols that enable the organoids to grow for long periods of time, achieving greater complexity and maturity than before. These organoids contain thousands of cells and multiple brain cell types that interact with each other in complex ways, making them excellent models for studying how neuropsychiatric or neurodevelopmental pathologies affect the ways brain cells talk to each other.
Already, researchers have been able to use organoids derived from autistic patients to show abnormalities in the regulation of genes involved in cell proliferation. Other researchers have used organoids to observe how the Zika virus associates with microcephaly during early embryo development, when it hinders normal brain development by driving the premature differentiation of neuron-producing cells. And others are looking at how these organoids, both “normal” and “diseased”, respond to certain stimuli.
Brain organoids will also bring insights into how the brain is formed during early development, something that has been studied for more than a century and still puzzles scientists. “The real goal right now is to use the organoids as disease models, but along the way I predict we are going to learn a lot about how the brain is formed,” Arlotta said.
Studying stem cell diseases and personalized medicine
Stem cells hold great promise as therapeutic tools due to their unlimited capacity to divide and regenerate tissue. But researchers are also realizing that many diseases might be caused by anomalies in the stem cells themselves or in the way other cells communicate with them.
Researchers like Carla Kim, PhD are using organoids to determine the role of stem cells in tissue regeneration, maintenance, and function and to understand how these cells talk to each other.
Kim and her group were the first scientists to grow lung organoids that mimic two distinct parts of the lung: the airways and the alveolar sacs where gas exchange occurs. They did it by using a special culture setup that allowed the cells to be in contact with both air and liquid, mimicking the lung environment. Their culture also included helper cells derived from blood vessels to stimulate stem cell growth.
“We want to know how does a stem cell know which type of specialized cells it has to make,” Kim said. Organoids help answering that question. “We are asking what factors and compounds need to be present to tell the stem cells what they need to grow.”
Kim uses a similar approach to study the reverse of that question: what happens in diseases where stem cells either fail at their job or create defective cells?
“Many lung diseases seem to us like a failure of stem cells, where they are not being able to repair damage,” said Kim. “For a long time, it’s been thought that diseases like emphysema could be caused by stem cell defects, but it has not been possible to test this idea. Now we can create organoids from diseased cells and conduct experiments to find out if stem cells or the helper cells that talk to them are at the cause of lung disease. If we are able to understand what goes wrong at the stem cell level, there could be a whole new cell type that could be a target for drugs.”
Organoids can also be used to screen directly for drugs that might enable the formation of a specialized cell type. That could help find treatments for diseases like cystic fibrosis, in which the ciliated cells that normally remove mucus from the lung are not working properly.
“We are able to make organoids with ciliated cells derived from patients and then test them for drugs that might make these ciliated cells work better,” Kim said. “We can make the organoids from iPSCs that are derived from the patient’s blood and try these patient specific lung cells without even taking a biopsy. With organoids the possibilities are endless. This is a very exciting time for studying the lung.”
Organoids as therapeutic tools
Several teams at Harvard and elsewhere are trying to come up with ways of transforming and transplanting cells, or even tissue, that could serve as a cure or treatment for certain diseases.
That is the case for HSCI scientist David Breault, MD, PhD who, along with another HSCI researcher, Qiao Zhou, PhD, has made groundbreaking advances in transforming intestinal cells into insulin producing beta cells. Their approach could lead to a treatment for diabetes, a large public health problem.
Diabetes is a metabolic disease related to insulin, a hormone made by the pancreas that allows our cells to absorb glucose from the bloodstream. There are two types of diabetes: type 1, in which the immune system attacks the insulin-producing beta cells; and type 2, in which cells become resistant to insulin, so the supply the body’s supply is not enough to control blood glucose levels.
Breault and Zhou developed a method to transform intestinal epithelial cells into insulin-producing beta cells and tested their method on intestinal organoids. This transformation is possible because these cells come from the same region during development and share many characteristics.
They were also able to show that they could implant a matrix loaded with these modified insulin-producing cells into a diabetic mouse, which then successfully regulated blood sugar levels.
Breault goes one step further and hints at the possibility of producing organoids from patient derived iPS cells that could be transformed into insulin-producing beta-like cells.
“The ability to make patient-specific progenitor cells that could be converted in perhaps one or two steps into beta cells might represent a significant advance in the treatment of diabetes,” Breault said.
A revolution in drug discovery
Not every research question needs to be answered using complex tissue-like cultures comprised of a diversity of cells.
Some scientists need only specific cell types that are similar to each other. One example is during the process of drug discovery, where numerous substances need to be tested on cells to see how they work.
To date, to conduct such tests the pharmaceutical industry has relied on animal models and human cell lines that have little resemblance to normal or diseased tissue. According to HSCI Executive Committee member Lee Rubin, PhD, that might be one of the reasons behind the high failure rate of clinical trials, adding to the high cost of drug discovery — an average of $2 billion for each new drug that reaches the pharmacy.
Rubin believes that using human cells rather than animal models could make the drug discovery and development process both faster and more effective.
Rubin’s lab is working on brain spheroids densely populated balls of neurons that consistently produce one type or a few types of cells in large quantities. This method produces more cells and with better quality than traditional flat cultures on a dish. It’s like a mass-production, economy-of-scale approach to cell culture.
In addition to development from embryonic cells, spheroids can also be derived from a patient’s own cells and deposited into a biobank of patient-specific cells. Combining such biobanks with clinical and genomic data, it might be possible devise and test individualized treatment plans for each patient. This approach could also allow the identification of groups of patients that might respond better to certain treatments than others.
Being able to produce a limitless supply of tissue from each patient will also be extremely useful to the study and treatment of rare diseases, where the number of patients on which to conduct research and test treatments is limited. This will allow researchers to conduct their research at a larger scale, accelerating progress in these often under-studied diseases.